What Lifestyle Practices Can Assist in Decreasing the Risk of Depression?
Research has demonstrated that living a healthy lifestyle involving social interaction, healthy sleep patterns, balanced nutrition, moderate alcohol consumption and regular physical activity while limiting sedentary behaviors and smoking reduces depression risk significantly.
Researchers studied multiple factors, such as brain structure, genetics, lifestyle factors and metabolic and immune systems to ascertain potential mechanisms that explain this relationship.
According to WHO data, nearly one out of twenty individuals suffer from depression – making this disorder an enormous public health burden globally. The factors responsible for initiating depression can include lifestyle and biological influences that play into its development.
To investigate the association between depression and these factors, data were drawn from the UK Biobank; an extensive research resource that contains participants’ health, lifestyle, and genetic details.
Researchers studied data collected on almost 290,000 individuals who experienced depression over 9 years and identified seven healthy lifestyle factors linked to reduced depression risk. These included:
Frequent social interaction, low to moderate sedentary behavior, not smoking and regular physical activity as well as moderate alcohol consumption are key elements for healthful lifestyle choices.
Sleep-Hygiene.
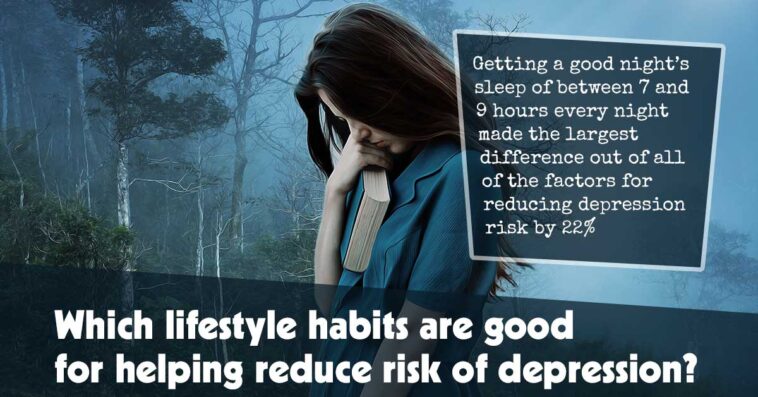
Of all of the factors studied, getting between 7 to 9 hours of quality restful sleep each night had the greatest impact on reducing depression risk by 22%; this included both treatment-resistant depression as well as single episodes.
Regular social contact proved the strongest protection from recurrent depression, reducing risk by 18% on average.
Nonsmokers were found to reduce depression risk by 20%; regular physical activity reduced it by 14%; low-to-moderate sedentary behavior reduced its risk by 13%; moderate alcohol consumption was linked with 11% reduction and eating healthily could further lower risks by 6%.
Individuals were divided into one of three groups depending on how many healthy lifestyle factors they complied with – favorable lifestyle, intermediate lifestyle or unfavorable lifestyle.
Intermediate group participants were 41% less likely to experience depression compared to unfavorable lifestyle individuals; favorable lifestyle individuals were 57% less likely.
Researchers next analyzed their DNA, assigning each participant a genetic risk score based on how many genetic variants have been linked with depression risk.
Individuals with lower genetic risk scores were 25% less likely to develop depression compared to individuals with the highest scores, although this had much smaller effects compared to lifestyle.
Researchers found that people at low, medium and high genetic depression risk could benefit from adopting healthy lifestyle practices to lower their depression risk.
These findings underscore the importance of leading a healthy lifestyle to prevent depression regardless of genetic risk factors.
Though our genes may increase our risk for depression, the study shows that leading a healthy lifestyle could be more essential.
Lifestyle factors can be under our own control and improving key aspects like getting out to socialize or making sure we get enough rest can make a significant impactful difference in people’s lives.
Researchers conducted several analyses in order to understand how leading a healthier lifestyle reduces depression risk.
Initial studies analyzed MRI brain scans from just under 33,000 individuals and discovered several brain areas where higher volume, defined as more connections and neurons, was associated with leading a healthier lifestyle, including amygdala, hippocampus, pallidum and thalamus.
Researches then looked for blood markers that indicated metabolic or immune system issues, including markers associated with lifestyle such as C-reactive protein produced in response to stress as well as one of the primary forms of fat used by our bodies for energy storage: Triglycerides.
Studies support these links between stress exposure and blood sugar regulation and immune function decline, leading to further age-related damage of molecules and cells within the body.
Sleep deprivation and inadequate physical activity can impede our bodies’ ability to respond effectively to stress, while insufficient social support or feelings of isolation have been shown to raise immune deficiency markers and raise risks of infection.
Researchers concluded that lifestyle was the single most influential factor when it comes to metabolic and immune function pathways; that is, poor lifestyle choices have an adverse impact on metabolism and immunity systems resulting in an increase in depression risk.